Everyday care in inpatient facilities is characterized by scarce resources and high time pressure. At the same time, the demands on quality, documentation, and individual care are increasing. Dealing with incontinence is particularly sensitive, as care needs, the dignity of residents, and economic aspects are closely interlinked. As a digital care assistance system, Alea addresses precisely this interface and uses digital technology to streamline processes, reduce stress, and manage care in a more targeted manner.
At the heart of Alea is digital incontinence management based on continuous measurement. A sensor detects the moisture level in the incontinence product and automatically transmits the data to software. Caregivers receive clear information about when a change is necessary and when it is not. This replaces manual visual checks, which previously often took place at fixed intervals – regardless of actual need. This approach is particularly relevant at night. Residents no longer have to be routinely woken up just to check for possible incontinence. Instead, the system indicates when action is actually needed. For those affected, this means undisturbed sleep, and for caregivers, it means noticeable relief and more confidence in their decisions.
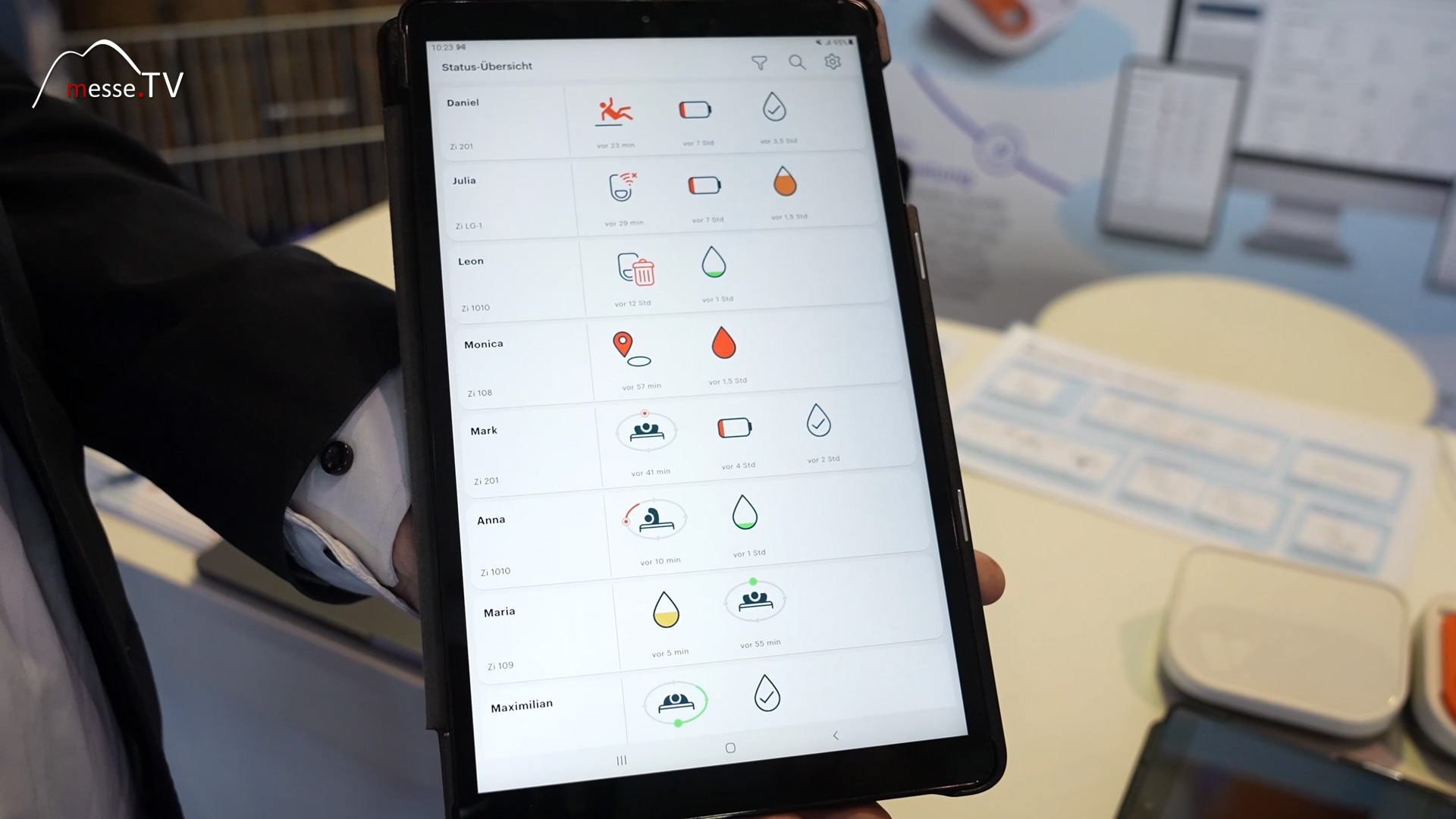
Alea is designed as an Internet of Things solution. Hardware and software form a closed system that processes data in real time. The information is displayed in an app that can be used on smartphones, tablets, or larger devices. Connection to existing home emergency call or ward systems is also planned. This modular structure facilitates integration into existing care processes. Facilities do not have to reinvent their processes, but can use digital support specifically where it brings the greatest benefit. At the same time, a traceable data basis is created that objectively supports care decisions.
In addition to incontinence detection, Alea also records movements in bed. An integrated sensor provides information about changes in position, activity, and prolonged inactivity. This results in two central areas of application: fall detection and pressure ulcer prevention. Caregivers can see whether residents are moving regularly or whether prolonged pressure loads are occurring. This means that positioning measures can no longer be planned on a blanket basis, but rather individually and in detail. This significantly reduces the risk of pressure ulcers. A single case of pressure ulcer can quickly cost nursing facilities tens of thousands of dollars—not to mention the strain on the individuals affected.

The effectiveness of the system was investigated in a large-scale study conducted in collaboration with the GKV-Spitzenverband (National Association of Statutory Health Insurance Funds). Over a period of around one and a half years, it was shown that the use of Alea can save around 25 percent in time and materials. Fewer unnecessary product changes, fewer leaks, and a more targeted use of incontinence materials have a direct impact on the use of resources. In addition, individual nursing homes have conducted their own cost-effectiveness analyses. These show that the costs of the system often pay for themselves after just six to nine months. This is based on savings in materials, working time, and follow-up costs that are avoided through preventive measures.
One of the key benefits of digital assistance is prioritization. Every day, caregivers are faced with the question of where their help is most urgently needed. Alea provides concrete information to help them answer this question. Instead of carrying out routine checks, they can focus their efforts on where care is actually needed. This not only improves efficiency but also job satisfaction. Decisions are based on data rather than assumptions. Especially in stressful phases, this creates confidence in one's actions and reduces unnecessary stress.
Digital systems only deliver sustainable benefits if they are affordable. That is why the question of reimbursement plays a central role. The available studies and analyses serve as a basis for discussions with nursing care insurance funds and for the development of viable reimbursement models. At the same time, it is clear that investments in digital nursing assistance cannot be viewed in isolation. Time savings, material reduction, and prevention work together. The result is a system that not only reduces costs but also stabilizes the quality of care.
Founded in Berlin in 2017, AssistMe has brought Alea to market maturity after several stages of development. A first generation of products was already tested before the pandemic, and delays were used to further develop the system on a scientific basis. The current version is based on real care processes and is specifically aimed at inpatient facilities. Alea is an example of a development in which digital nursing assistance is not seen as a replacement for human work, but as a tool to ease the burden. Technology takes care of measurement and information, giving nursing staff more time for care and professional decisions.
The Alea nursing assistance system shows how digital solutions can have a concrete impact in everyday life. It combines incontinence management, movement tracking, and preventive care into an integrated approach. The decisive factor here is not the technology itself, but its usefulness in daily operations. In an industry under structural pressure, digital assistance can help to ensure quality and make sensible use of resources. Alea provides an example of this based on data, studies, and practical application—and thus goes far beyond pure theory.